Langley (604)-530-1561
Fax (778)-278-1561
Email podiatry@urton.ca
July 2021
Bunionettes: The Pinky Toe Bunions
 You may have heard of bunions, which sometimes pop up at the base of the big toe joint, but what is a bunionette? Bunionettes, also known as tailor’s bunions, are small, bony bumps that occur at the base of the pinky toe joints. Much like regular bunions, bunionettes can be painful, swollen, and red. Finding comfortable shoes that don’t rub up against the affected area may be difficult. Without treatment, bunionettes usually worsen over time. Fortunately, conservative treatments such as wearing wider shoes, a toe spacer, padding, and activity modifications, are often effective in managing the condition. Surgery to correct a bunionette may be beneficial for a smaller percentage of people. To learn more about bunionettes and what treatment methods are best for you, please consult with a podiatrist.
You may have heard of bunions, which sometimes pop up at the base of the big toe joint, but what is a bunionette? Bunionettes, also known as tailor’s bunions, are small, bony bumps that occur at the base of the pinky toe joints. Much like regular bunions, bunionettes can be painful, swollen, and red. Finding comfortable shoes that don’t rub up against the affected area may be difficult. Without treatment, bunionettes usually worsen over time. Fortunately, conservative treatments such as wearing wider shoes, a toe spacer, padding, and activity modifications, are often effective in managing the condition. Surgery to correct a bunionette may be beneficial for a smaller percentage of people. To learn more about bunionettes and what treatment methods are best for you, please consult with a podiatrist.
If you are suffering from bunions, contact William Urton, DPM of British Columbia. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
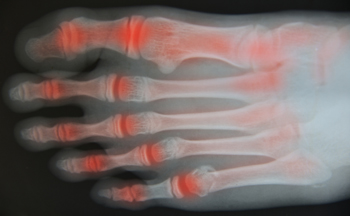
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Langley, BC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Signs of Cuboid Syndrome
 The cuboid is a cube-shaped bone located in the middle of your foot. This bone can become injured or dislocated following an injury to the foot. People who play sports that put a lot of stress on the feet and people with notable overpronation of the feet are said to have an increased risk for developing this condition. The most common symptom of cuboid syndrome is pain and weakness in the affected foot, particularly when bearing weight. The foot may also be swollen, tender, or red. These symptoms can be severe enough to make walking or standing difficult, sometimes causing a limp, and interfering with daily activities. Symptoms can also have a sudden or gradual onset. If your foot is showing any signs or symptoms of cuboid syndrome, it is suggested that you consult with a podiatrist as soon as possible.
The cuboid is a cube-shaped bone located in the middle of your foot. This bone can become injured or dislocated following an injury to the foot. People who play sports that put a lot of stress on the feet and people with notable overpronation of the feet are said to have an increased risk for developing this condition. The most common symptom of cuboid syndrome is pain and weakness in the affected foot, particularly when bearing weight. The foot may also be swollen, tender, or red. These symptoms can be severe enough to make walking or standing difficult, sometimes causing a limp, and interfering with daily activities. Symptoms can also have a sudden or gradual onset. If your foot is showing any signs or symptoms of cuboid syndrome, it is suggested that you consult with a podiatrist as soon as possible.
Cuboid syndrome, also known as cuboid subluxation, occurs when the joints and ligaments near the cuboid bone in the foot become torn. If you have cuboid syndrome, consult with William Urton, DPM from British Columbia. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Cuboid syndrome is a common cause of lateral foot pain, which is pain on the outside of the foot. The condition may happen suddenly due to an ankle sprain, or it may develop slowly overtime from repetitive tension through the bone and surrounding structures.
Causes
The most common causes of cuboid syndrome include:
- Injury – The most common cause of this ailment is an ankle sprain.
- Repetitive Strain – Tension placed through the peroneus longus muscle from repetitive activities such as jumping and running may cause excessive traction on the bone causing it to sublux.
- Altered Foot Biomechanics – Most people suffering from cuboid subluxation have flat feet.
Symptoms
A common symptom of cuboid syndrome is pain along the outside of the foot which can be felt in the ankle and toes. This pain may create walking difficulties and may cause those with the condition to walk with a limp.
Diagnosis
Diagnosis of cuboid syndrome is often difficult, and it is often misdiagnosed. X-rays, MRIs and CT scans often fail to properly show the cuboid subluxation. Although there isn’t a specific test used to diagnose cuboid syndrome, your podiatrist will usually check if pain is felt while pressing firmly on the cuboid bone of your foot.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are ice therapy, rest, exercise, taping, and orthotics.
If you have any questions, please feel free to contact our office located in Langley, BC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Cuboid Syndrome
Cuboid syndrome mostly affects athletes, although it can affect non-athletes too. It is also known as cuboid subluxation or cuboid fault syndrome. This condition occurs when joints and ligaments near the cuboid bone of the foot are damaged, or when the cuboid bone itself is dislodged from its natural position. It is usually marked by pain on the outer side of the foot, which may be persistent or may come and go. Cuboid syndrome can be difficult to diagnose unless it becomes severe and more noticeable. Your doctor will likely ask questions about when the pain began and how long it has been present, and will put pressure on the cuboid bone to determine if that area is the origin of the pain.
Causes of Cuboid Syndrome
- Any repetitive stresses placed on the foot due to athletic activities are a common cause of cuboid syndrome.
- Although it develops over time, it is possible that this syndrome can occur all of sudden due to a single event or injury.
- Over-pronation can exacerbate the condition if not corrected.
Disagreements Amongst Podiatrists Regarding Cuboid Syndrome
- Some refer to it as the dislocation of the calcaneal-cuboid joint only.
- Other podiatrists see it as an injury of the ligaments located nearby, which also involves the cuboid bone.
It is very important that when you experience any kind of pain on the side of your foot, you should seek medical care right away. If a subluxed cuboid is caught early, your feet may respond well to the treatment, and you can get back into sports or other activities again as soon as the pain subsides.
Why Live with Pain and Numbness in Your Feet?
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
The Most Common Cause Of Heel Pain
Heel pain is a common ailment which may be caused by an irritation of the nerves, arthritis, tendonitis, stress fractures in the heel, a cyst, or—most commonly—plantar fasciitis. Plantar fasciitis occurs when the plantar fascia—the long band of connective tissue on the sole which links the heel bone to the toes—becomes torn, stressed, or otherwise damaged. Repetitive movements during sporting activities, having flat feet or high arches, obesity, prolonged standing, non-supportive footwear and other factors can all put undue stress on the plantar fascia and cause this painful condition to manifest. If you have heel pain of any kind, make an appointment with a podiatrist who can pinpoint the cause of your heel pain and treat it accordingly.
Many people suffer from bouts of heel pain. For more information, contact William Urton, DPM of British Columbia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Langley, BC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Arthritic Foot Care
During your lifetime, you will probably walk about 75,000 miles, which is quite a lot of stress to put on your feet. As you get older, the 26 bones and 30 joints in each of your feet will lose flexibility and elasticity. Your foot’s natural shock absorbers will wear down as well. Having arthritis added to this mix only makes matters worse. Your joints will become distorted and inflamed, which is why arthritic foot care needs to be something to think about every day.
When dealing with arthritis, having additional foot complications, such as bunions, hammertoes, or neuroma, can be a serious detriment. To avoid these, buy well-fitting shoes with a lower heel and good support. Arthritis causes you to lose your arch, so having shoes with good arch support is also highly recommended.
Aside from getting good arch support, the shoes need to fit comfortably and properly as well. A good place to start is by leaving a finger width between the back of the shoe and your foot to gauge proper size. It is also helpful to have a square or rounded toe box in the front to provide even more comfort. Another thing to look for is a rubber sole that can provide a cushion and absorb shock as you walk. This adds flexibility to the ball of your foot when you push off your heel to walk.
Exercise is another key aspect of arthritic foot care. Exercise not only strengthens and stretches your muscles and joints, but helps to prevent further injury and pain as well. Stretching the Achilles tendon, the tendon located in the back of your heel, will give you added mobility and reduce pain due to stress. Another thing you can do is massage your feet, kneading the ball of your foot as well as your toes from top to bottom.
Stretching the Achilles tendon is a simple exercise that you can do at home anytime. Lean against the wall with your palms flat against the surface while placing one foot forward, towards the wall, and one foot behind you. Bend your forward knee towards the wall while keeping your back knee locked straight, and make sure both your heels are completely touching the ground at all times. This will stretch your Achilles tendon and calf muscles as well. You will feel the stretch almost immediately. You can also stretch your toes in a couple ways. One involves taking a rubber band and wrapping it around both your big toes while your heels remain together. Then, pull them apart to stretch your big toe. You can also place a rubber band around all the toes of one of your feet. Then, try to separate each individual toe, stretching them all.
A final step you can take to help your arthritis is taking non-steroid, non-inflammatory drugs or topical medicines with capsaicin. Unfortunately, there is no complete way to remove all of your arthritic pain. However, following some of this advice can go a long way in staying as pain-free as possible.
What Are the Early Signs of Foot Arthritis?
We often associate arthritis in the feet with aging, but there are many types of arthritis that can strike at any age. Osteoarthritis tends to be one of the more common conditions people are familiar with. This form of arthritis is caused by age-related degeneration of the cartilage between the joints. Rheumatoid arthritis on the other hand, is an autoimmune disorder that can affect young children. Gout, which is known for its sudden and very painful periodic flare ups, is also a type of arthritis. Generally, the early signs of arthritis in the feet include joint stiffness, pain, swelling, and warmth. The joints may also become deformed. Mucous cysts can sometimes form at the ends of the toes or underneath the toenails, and knobby growths called bone spurs may develop on the heels. If you detect any symptoms of arthritis in your feet, it is suggested that you seek the care of a podiatrist.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact William Urton, DPM from British Columbia. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Langley, BC . We offer the newest diagnostic and treatment technologies for all your foot care needs.